The subtitle of a Wall Street Journal article from July 2011 asks a question a personal injury lawyer hears nearly every day from insurance claims adjusters and defense attorneys. “Doctors Challenge: How Real Is That Pain?” explains that “despite decades of research, doctors have few tools to measure pain objectively. Generally, they ask patients to rate it themselves from one to 10, or point to the cartoon face on the wall chart whose expression best matches how they feel.”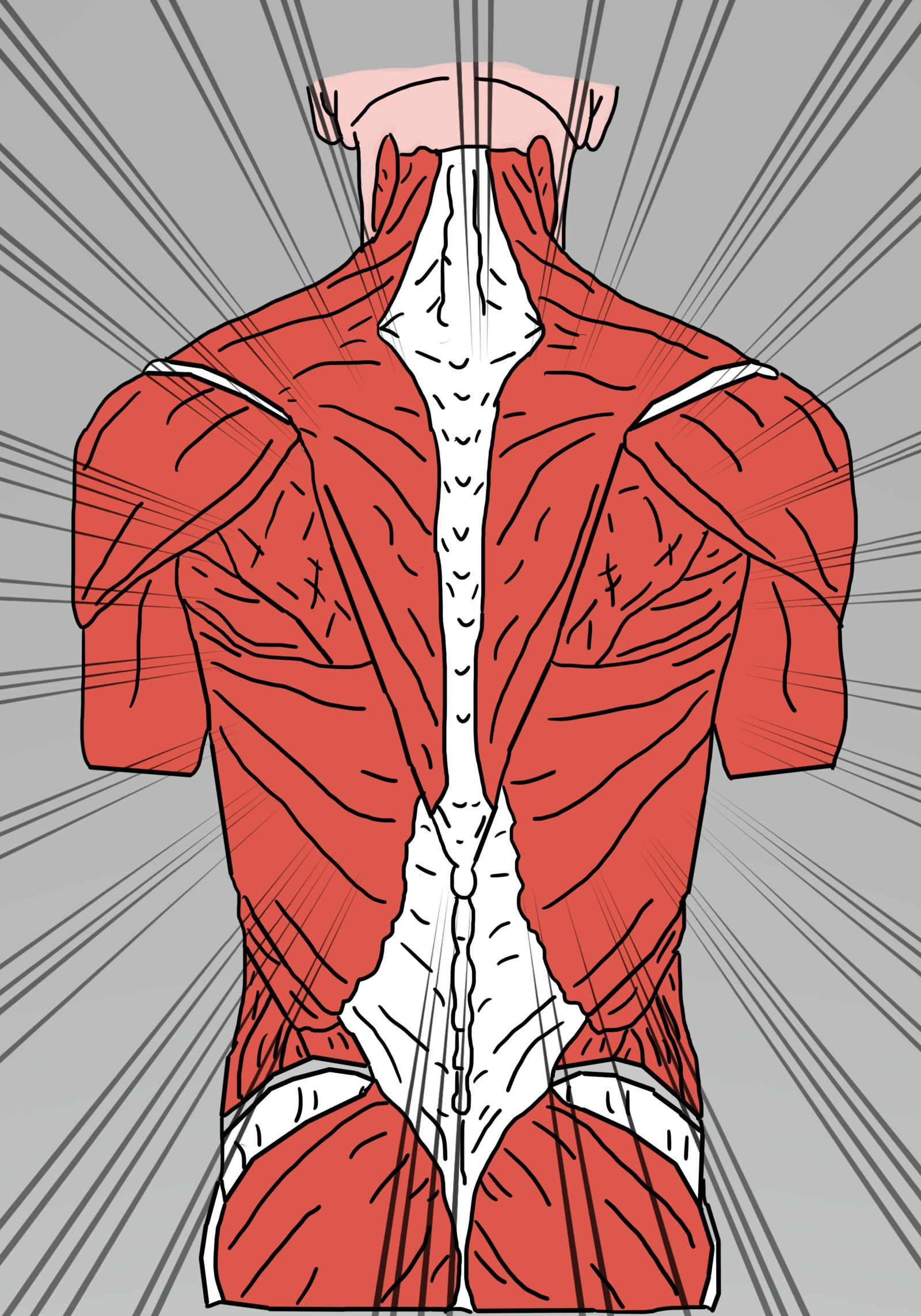
Such self-reports lead even medical professionals to conclude that some percentage patients are faking. A further problem is that physicians and nurses were taught for centuries that Black people and children are less sensitive to pain than are white adults.
Even when reports of pain are believed, knowing how to provide relief can be difficult. Locating the source of pain and accurately describing the mechanism by which pain signals are being generated often eludes the most-expert health care providers. Further, stress and depression can affect how people perceive and respond to pain. Emotional distress can heighten sensitivity to pain, and being in pain often creates emotional distress.
LEARN MORE
- What Is Preponderance of the Evidence?
- What Noneconomic Damages Can a Virginia Personal Injury Victim Claim?
- How a Virginia Personal Injury Attorney Proves an Accident Caused or Worsened a Herniated Disc
The truth is that pain is very real. The problem, from the standpoint of health care and personal injury law, is that each individual, regardless of race or age, has a different threshold for how much physical discomfort they can ignore while continuing to go about living their lives, working, playing and enjoying themselves.
Unfortunately, pain remains poorly treated because few generally available therapies work well for everyone. The deadly dangers of opioid painkillers such as Vicodin (hydrocodone) and OxyContin (oxycodone) are well recognized. But those medications do have legitimate uses for controlling acute pain immediately following surgery and breakthrough pain from late-stage cancer. They just are not appropriate for the large majority of people with long-term or chronic pain.
Over-the-counter medications can cause liver and kidney damage when taken at the high doses needed to minimize serious pain. Physical therapy and other nonpharmaceutical interventions can help, but pain produced by chronic or degenerative conditions will eventually worsen to the point that only drugs will help.
Which brings the actual questions raised by the WSJ article and those who would deny compensation to personal injury victims into focus; namely,
- How can pain be real if it is different for everyone?
- Why should anyone believe self-reports of the severity and persistence of pain?
- Even if the pain does exist, why should it be considered disabling and debilitating?
- Since we know pain is, to some extent, a mental sensation, couldn’t it all be in the person’s head?
A very strong rebuttal to several of these dismissals of pain sufferers is that things people think and feel are quite real to them. But that bit of logic will not win an argument in front of an arbiter or judge while trying to secure a settlement for a personal injury victim.
Medical Evidence Matters as Much as Testimony
Personal injury settlements and awards from juries in civil lawsuits typical have two components. Economic damages represent payments for the direct, calculable costs of an injury that was caused by someone else’s negligence or recklessness. Hospital and therapy bills, lost wages and loss of future income due to disability are economic damages.
Noneconomic damages represent compensation for physical pain, emotional distress and mental anguish. In other words, noneconomic damages are the awards for the pain and suffering an injury victim experiences as a result of someone else’s negligence or recklessness.
To prove that our clients experienced pain, my Virginia Beach-based personal injury law firm colleagues and I first rely on medical evidence. X-rays that show broken bones, MRIs indicating pinched nerves and herniated spinal discs, and notes made by treating physicians in a patient’s medical record all constitute strong evidence that our client was or remains in pain. Expert testimony from neurologists and psychologists also helps us prove pain claims.
In addition to the objective evidence, we take official statements from spouses, family members, friends and coworkers who possess firsthand knowledge of our client’s situation before and after the injury. Detailed descriptions of how pain interrupted or continues to complicate a person’s life can be powerful.
EJL