RESULTS: $2.23 Million Wrongful Death/Medical Malpractice Verdict (Delayed Diagnosis of Hospital Sepsis)
COURT: Norfolk, VA Circuit Court
DATE: April 2023
ATTORNEYS: Richard N. Shapiro, Eric K. Washburn
STAFF: Paula S., Heather G.
“Our family had a tragedy that was unexpected, terrible and life-changing and if anybody asks for a recommendation, I will without hesitation recommend Mr. Shapiro, Mr. Washburn, and their law firm. They are a fantastic team, fantastic representation, their support was huge every step of the way. I honestly feel as if this firm, these people, are in my personal circle now.” – Hannah B.
WHAT HAPPENED:
In 2018, a 58-year-old nurse was employed at DePaul Hospital in Norfolk, VA, and had been working for five years in the neurosurgical operating suite at the hospital. She developed strange abdominal pain and was seen by one of the surgeons with Bon Secours Surgical Specialists, who recommended she undergo a colon resection surgery to remove part of her colon.
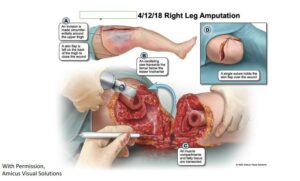
4/12/18 Right Leg Amputation
The colon surgery took place on April 4, 2018, and was uneventful. But on April 14, our client died at DePaul Hospital, following several post-operative surgeries, involving re-exploration of the abdomen, wound debridement, and finally a right leg amputation, all due to the effects of septic shock and fast-spreading necrotizing fasciitis infection.
Before trial, her surgeon admitted a leak had formed from the resected colon/intestinal area, which spewed fecal contents into our client’s abdominal cavity for a number of days and ultimately trailed down the abdominal cavity to her right thigh, developing into necrotizing fasciitis. Nonetheless, the surgeon and her surgical colleague, who rounded on our client, both denied any negligent responsibility and denied any unreasonable delay in medical standards of care before recognizing her infection and its consequences.
LEGAL STRATEGIES
As attorneys for the nurse’s family and estate, we subpoenaed all medical records, including the electronic “audit trail” of electronic patient records accessed by her providers. The hospital and surgeons refused all pre-suit settlement overtures.
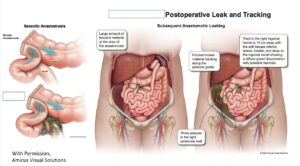
Postoperative Leak and Tracking
During litigation, careful review of the hospital records revealed that the surgeons ordered a blood test on April 8, postoperative day four, which showed highly abnormal band neutrophils, a part of the white blood cells that always spike when the body fights a new infection. Despite the abnormal results, the surgeons never initiated an antibiotic, nor obtained an abdominal CT scan which likely would have lit up and shown fecal contents were leaking into the nurse’s abdomen over several prior days. The surgeons even repeated a CBC blood test a day later, on April 9, showing that the “bands” had skyrocketed higher, to nine times over normal.
During relevant depositions, we contended the surgeons didn’t recognize sepsis for 36 to 48 hours when all physicians agreed every hour of antibiotic administration can make a huge difference in the survival of a septic patient.
The medical record audit trail showed one of the two surgeons had accessed the results of the blood tests on each day they were returned but had either never appreciated the “band” count nor acted to medically intervene with urgency as to the highly abnormal “band” results.
Plaintiff’s medical experts, two surgeons, each testified results of the blood tests on April 8 and 9 would have caused a reasonably prudent surgeon to immediately order an abdominal CT scan, start antibiotics, and likely do immediate exploratory surgery, but the surgery did not occur until two calendar days later.
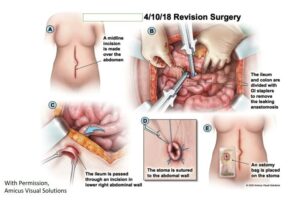
4/10/18 Revision Surgery
We also retained an infectious disease doctor, who testified had he been consulted after the first blood test results, he would have suspected septic infection, begun antibiotics on the patient, requested an abdominal CT scan, and urged the attending surgeon to do immediate exploratory surgery for an intra-abdominal leak.
Besides creating detailed timelines and charts synthesizing the key medical evidence, we also supervised the creation of professional medical illustrations to document the many surgeries the nurse underwent before she succumbed to septic shock on April 14, and presented the testimony of the pathologist and her autopsy results, which confirmed multi-organ failure due to septic shock and necrotizing fasciitis. We called 18 witnesses in total at trial and the defense called six, including surgeons and an infectious disease doctor who fully defended the surgeons.
THE RESULTS: $2.23 million

The victim’s daughters with Attorneys Rick Shapiro and Eric Washburn
Following the five-day Norfolk, VA medical malpractice/wrongful death jury trial, the jury deliberated nearly five hours before returning a $2.23 million verdict in favor of our client’s estate, comprised of her twin 31-year-old daughters. The highest defense settlement offer made the week before was $750,000, which was withdrawn after it was declined.
